Embryo Grading – Quality Chart and IVF Success Rates
Embryo grading is a visual assessment technique carried out by an embryologist which helps choose the best embryos for further transfer within an IVF program.
During IVF embryologists evaluate and classify embryos every day based on specific criteria and create an embryo grading chart. It takes 6 days (0-6) and is usually done twice – on days 3 and 5. The retrieval day is considered a day zero.
Right after the retrieval, they collect oocytes and this is where the processes can differ for traditional IVF where oocytes meet sperm in a petri dish, and ICSI, where washed sperm is injected into an egg with a micro-needle. Let’s take a closer look at embryo grading during IVF and ICSI.
IVF Fertilization
IVF embryo grading starts with a visual analysis of the oocyte-cumulus complex (OCC). It cannot give complete certainty to judge the maturity of oocytes, since oocytes are not cleared of cumulus cells for such fertilization.
- If the OCC looks dense and dark, then the embryologist rates it as “0”.
- If the OCC looks loose and transparent, then it usually contains a mature oocyte and receives a score of “1”.
- If the next day, after cleaning the oocytes from cumulus cells and checking fertilization, this oocyte was indeed mature, the score looks like “1–1”.
- If the oocyte turned out to be immature, the score is “1–0”.
ICSI Fertilization
This assessment is done one hour after receiving the OCCs, which are processed with an enzyme to separate oocytes from excess cells. In this case, the embryologist can confidently define the number of mature (suitable for fertilization) oocytes and fertilize them with sperm via injection.
- Column 0 is the day of the puncture (day zero).
- OOC stands for the oocyte-cumulus complex.
- MII – Mature oocyte.
- MI, GV – Immature oocytes (not suitable for fertilization, MI stage oocytes can mature in a petri dish, but zygotes obtained after such fertilization, usually do not give good embryos).
- ABN – abnormal oocytes (which are not suitable for fertilization. They can be without a membrane, have inclusions in the cytoplasm, irregular shape, etc. They may be both mature and immature).
- ATR – atretic (degenerative) oocytes (not suitable for fertilization).
Embryologists fertilize only MII (metaphase oocyte II).
Only good oocytes are suitable for fertilization
The embryologist monitors the action literally by the clock, because various abnormal developmental variants are possible, which are monitored and cultivated separately. 16–18 hours after fertilization, specific rounded structures, pronuclei (PN), appear in the oocyte. These are precursors of the nuclei, containing the genetic makeup of both mom and dad.
Oocytes (NF – not fertilized, 1PN – fertilized with 1 pronucleus at day 1) are deposited separately and observed. If an excellent embryo is obtained from such an oocyte, then the reproductologist, embryologist, and patient decide to transfer or freeze it.
Further development of the embryo, crushing, occurs within 6 days.
- 2PN – two pronuclei (normal fertilization). These embryos are cultivated further.
- NF – no pronuclei. Fertilization either occurred, but the pronuclei disappeared too quickly, or the oocyte was not fertilized.
- 1PN – one pronucleus. In 25% of cases with 1PN, the embryo can be diploid.
- NS – the oocyte did not survive after the ICSI procedure.
- 3PN or more – an abnormal embryo. The transfer of such an embryo is prohibited; such embryos are never used in the clinic.
Single Culture Media
For the cultivation of embryos in the clinic, advanced single-culture media are used, which allow you to leave the embryos alone until the 5th day of development.
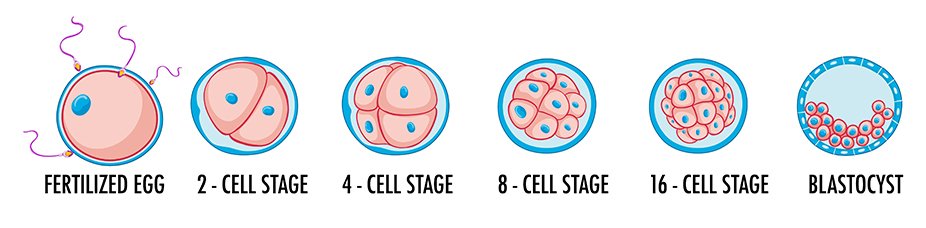
A day later, the embryo already consists of 6–8 blastomeres. Up to this point, the embryo has developed exclusively on the maternal reserves accumulated in the egg during its growth and development in the ovary. However, if the genetic program, which encodes the stages of normal development of the embryo, contains errors, the embryo (4-19% of cases) stops developing before reaching the blastocyst stage. It is a so-called developmental block, is a natural selection process for genetically normal embryos.
The most accurate assessment of embryos occurs at the blastocyst stage (5–6 days after fertilization). And if the best blastocyst grows out of the worst oocyte, it still has the maximum chances for successful IVF. Therefore, it is necessary to wait and give chance to all embryos.
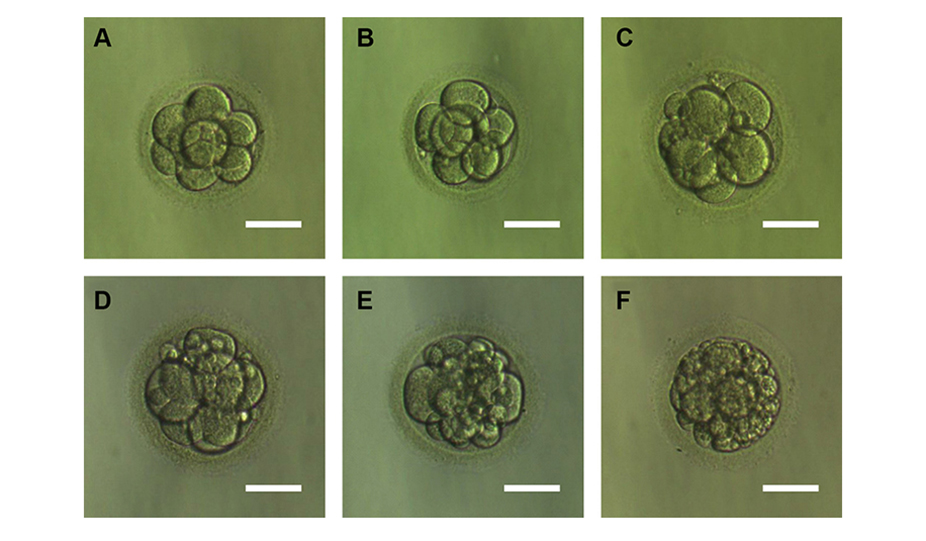
Embryologists use a numerical-alphabetic system for embryo grading (embryo quality assessment), where the first digit means the number of blastomeres, the letter is their quality, and the second digit is an estimate of fragmentation.
- Type A1 – an embryo with equal blastomeres, of excellent quality without anuclear (non-nuclear) fragments (for example, 4A1 – is a four-cell embryo with an excellent score).
- Type B2 – good quality embryo with up to 20% anuclear fragments (4B2)
- Type C – the embryo of satisfactory quality with the content of anuclear fragments from 21% to 50% (4C3)
- Type D – poor-quality embryo with more than 50% anuclear fragments (4D4)
Day 3 Embryo Grading Chart (D3)
| Grade | Fragmentation |
|---|---|
| A | No fragmentation or up to 10% |
| B | 25-50% fragmentation |
| C | More than 50% fragmentation |
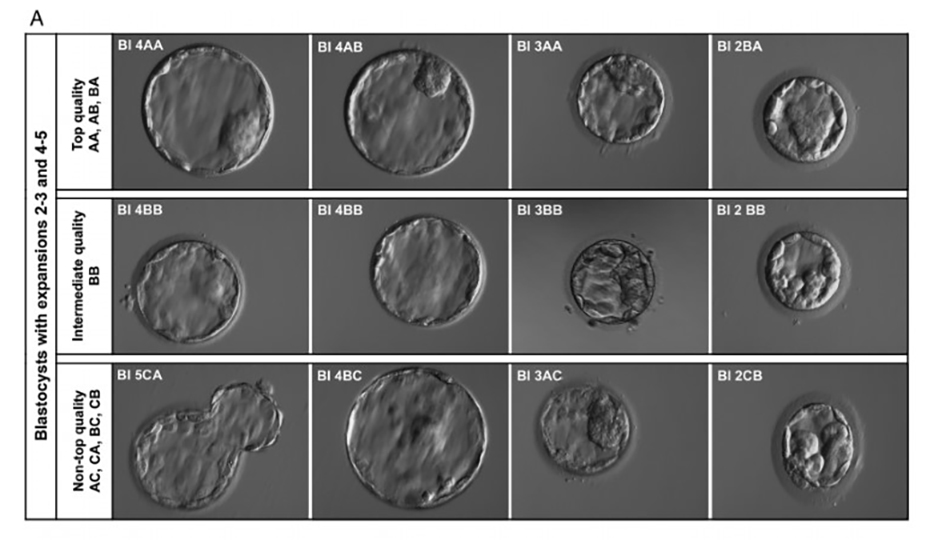
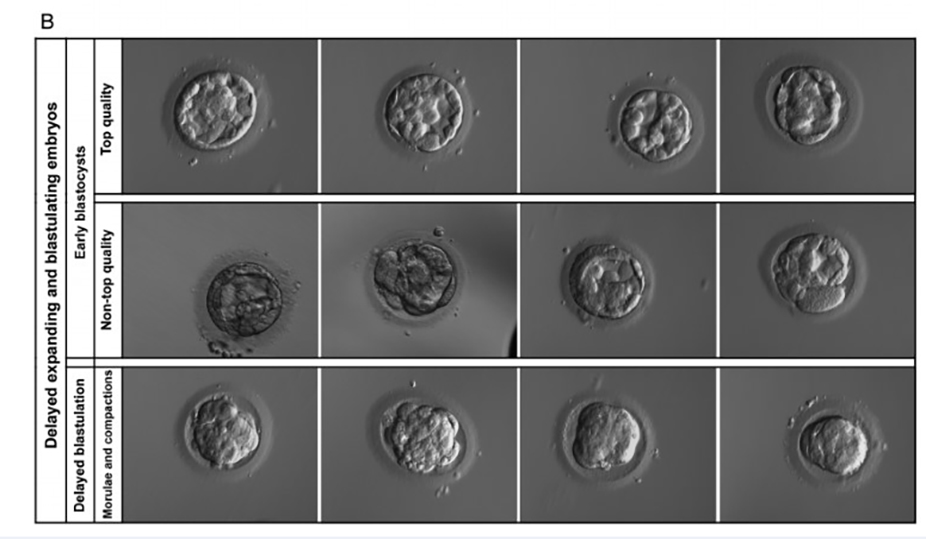
Classification of Blastocytes
Blastocyst grading takes place on day 5 according to the Gardner and Schoolcraft scoring system. It evaluates three main factors: the degree of blastocyst expansion (the cavity), inner cells (it will make the baby), and the outer part (trophectoderm that will make the placenta).
Blastocyst Embryo Grading – Numbers
When classifying blastocysts, the blastocyst expansion indicates a number from 1 to 6 (degree of development of the embryo):
- the blastocyst cavity is smaller than half of the whole embryo;
- the blastocyst cavity is bigger than half of the whole embryo;
- complete blastocyst, the cavity fills almost the entire embryo;
- developed blastocyst, the cavity includes the entire embryo, a thin shell;
- the blastocyst breaks out of the shell;
- blastocyst without membrane.
Inner Cells – Letter Designation
The quality of the intracellular mass from which the embryo will develop:
- A – many cells, densely packed;
- B – several cells, loosely grouped;
- C – very few cells.
Outer Cells – Letter Designation
The quality of the trophectoderm (TE) that will ensure the attachment of the embryo to the endometrium and development into the placenta
- A – many cells, form a single layer;
- B – few cells, form free epithelium;
- C – very few large cells.
Embryo Grading and Success Rates
| Blastocyst Expansion | ecxellent inner cell mass & ecxellent prophectoderm | ecxellent inner cell mass & good prophectoderm | good inner cell mass & good prophectoderm | good inner cell mass & poor prophectoderm | poor inner cell mass & poor prophectoderm | |
|---|---|---|---|---|---|---|
| cavity is smaller than half of the embryo | 1 | 1AA | 1AB | 1BB | 1BC | 1CC |
| cavity is bigger than half of the embryo | 2 | 2AA | 2AB | 2BB | 2BC | 2CC |
| cavity fills almost the entire embryo | 3 | 3AA | 3AB | 3BB | 3BC | 3CC |
| developed blastocyst, thin shell | 4 | 4AA 63-65% success rate | 4AB | 4BB | 4BC | 4CC |
| blastocyst breaks out of the shell | 5 | 5AA 60-65% succes rate | 5AB | 5BB | 5BC | 5CC |
| blastocyst without membrane | 6 | 6AA | 6AB | 6BB | 6BC | 6CC |
Frequently Asked Questions about Embryo Grading
Embryo grading is the process of embryo evaluation that takes place during the first 6 days after oocyte fertilization and lasts until the embryo transfer or freezing. The grading of the embryos for natural IVF and ICSI (Intracytoplasmic sperm injection) is different.
Embryologists consider embryos with grades 4AA and 5AA as excellent and morphologically perfect on day 5. However, embryos with lower scores can be also suitable for embryo transfer. E.g B-graded embryos have high pregnancy success chances.
Embryo grading during FET has the same importance as in the natural cycle. Embryologists choose only grade-A embryos for freezing. Therefore, embryo grading for frozen embryo transfer is extremely important.